Is partial response good enough?
Major depression among adults in the US has continued to increase1


Of an estimated 22 million US adults affected, approximately half, or 11 million, may not fully respond to their antidepressant2,3,a


has been defined as a 25-50% reduction from baseline in depression scale scores4,b
MDD symptoms reported by adult patients on one or more antidepressant5
Despite evidence supporting appropriate use, a chart review study showed that a patient may undergo ~5 treatment changes before being prescribed an adjunctive atypical antipsychotic6
Antidepressant treatment changes may affect response rates. In the STAR*D study, rates of response decreased with each additional switch in antidepressant treatment (48.6% in Step 1 to 16.3% in Step 4)2,d
Atypical antipsychotics may increase response rates for patients
According to a meta-analysis,
The chance of response doubled in patients treated with adjunctive atypical antipsychotics vs antidepressant treatments alone (odds ratio=1.68)7,e
aDemonstrated in almost 3700 adult patients with MDD who were prescribed an SSRI. In the STAR*D study, inadequate response was defined as less than 50% reduction from treatment step entry in QIDS-SR16 score at 12 to 14 weeks. Statistic is an extrapolation of the STAR*D study.2
bThe HAM-D has been the metric of choice for measuring depression in research settings. Other scales such as the MÅDRS and the Inventory for Depressive Symptomatology have also been used.4
cBased on an online survey of adult patients (n=2096) age 18-65 with an inadequate response to an antidepressant who reported symptoms occurring (1) several days to (3) nearly every day on the PHQ-9; current symptoms of depression were assessed with a modified PHQ-9 that excluded the question of suicidal ideation; non-PHQ-9 symptoms were elicited from a checklist of clinical symptoms associated with depression. In the survey, 38% of participants were taking combination antidepressant therapy (more than one antidepressant at the same time) and 16% were taking adjunctive atypical antipsychotics.5
dAs demonstrated in almost 3700 adult patients with MDD who were prescribed antidepressants. In the STAR*D study, partial response was defined as a less-than-50% reduction from treatment step entry in Quick Inventory of Depressive Symptomatology Self-Report score at 12-14 weeks. The patient sample received successive acute treatment steps: 3671 patients entered at Step 1; 1439 patients continued at Step 2; 390 patients proceeded to Step 3; 123 patients advanced through all 4 steps. After SSRI monotherapy in Step 1, treatment options included switching medications or augmentation with either medication or cognitive therapy. Adjunctive atypical antipsychotics were not included at any step. Patients who either did not achieve response with a treatment or were unable to tolerate a treatment were encouraged to move to the next step.2
eIn a meta-analysis, response was defined as a 50% improvement from baseline to endpoint on either the MÅDRS or HAM-D17. Meta-analysis included 17 randomized trials with 3807 patients (duration range: 4-12 weeks) comparing adjunctive antipsychotic treatment to SSRI/SNRI treatment in adult patients (age range: 18-65 years) with MDD. There was a 68% greater chance of response from the antidepressant + adjunctive antipsychotic group vs the antidepressant + placebo group.7
HAM-D17, 17-item Hamilton Depression Rating Scale; MÅDRS, Montgomery-Åsberg Depression Rating Scale; MDD, major depressive disorder; PHQ-9, Patient Health Questionnaire-9; QIDS-SR16, Quick Inventory of Depressive Symptomatology-Self Report 16; SNRI, serotonin and norepinephrine reuptake inhibitor; SSRI, selective serotonin reuptake inhibitor; STAR*D, Sequenced Treatment Alternatives to Relieve Depression.
Watch Dr. Jain discuss the prevalence of partial response
in MDD and considerations for addressing it
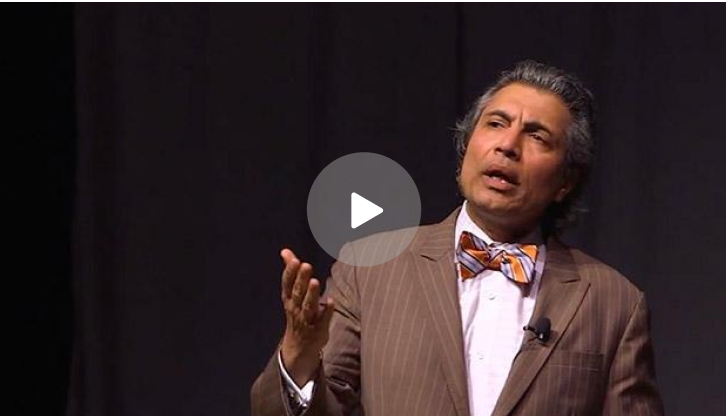
Rakesh Jain, MD, MPH
Clinical Professor
Department of Psychiatry
Texas Tech University School of Medicine
Austin, Texas
The presenter is a paid consultant of Otsuka America Pharmaceutical, Inc. and Lundbeck.
Review treatment history data for patients with MDD experiencing partial response to antidepressants, and learn about REXULTI as an adjunctive treatment option.
